Sexually transmitted diseases (STDs) are some of the most common health concerns in the United States. These infections are caused by pathogens like viruses, bacteria, or protozoans. They are treated with a range of medications. (Learn more)
Millions of new STD infections are recorded every year in in the U.S. Each of these diseases has a different approach to treatment, depending on the pathogen that causes it. (Learn more)
While each STD may have a different drug or treatment that works best for it, there are a few common steps you can take to reduce your risk of contracting an STD or preventing transmission at all. (Learn more) Understand your personal risk of STD infection and how you can best manage your sexual health. (Learn more)
What Are STDs & How Common Are They?
Sexually transmitted diseases (STDs) are bacteria, viruses, or other pathogens that are passed from one person to another through sexual contact. There are many types of STDs, and treatment can be very different, depending on the pathogen that causes the disease.
While there are several medical approaches to treatment, from antibiotics to immunosuppressant drugs, there are some recommended steps to prevent transmission of these diseases.
STDs are transmitted through sexual activity, including oral contact, vaginal penetration, or anal penetration. According to the Centers for Disease Control and Prevention (CDC), there are an average of 20 million new cases of STDs every year in the United States. Around half of these, or approximately 10 million cases, occur in adolescents and young adults, ranging in age from 15 to 24.
While young people may be more at risk, anyone who has unprotected sex is at risk of contracting an STD.
Most Common Types of STDs & Their Medical Treatments
Below are the most common STDs in the U.S. Depending on the pathogen causing the disease, treatment approaches may be very different.
- Bacterial vaginosis (BV): This is the most common STD among women between the ages of 15 and 44. Typically, the vagina maintains a balance of yeast and bacteria. Bacterial vaginosis is caused by a change in that balance, so there is too much bacteria.Currently, medical researchers do not know the exact cause of BV, but it is more likely to occur in sexually active women, although this is not fully understood. Symptoms of BV include:
- A thin, white or gray vaginal discharge.
- Pain, itching, or burning sensations in the vagina.
- A strong fish-like odor, particularly after having sex.
- Burning when urinating.
- Itching around the outside of the vagina.
Sometimes, bacterial vaginosis will go away on its own, as the vagina restores the balance between bacteria and yeast. However, treatment from medical professionals is the best way to clear this disease. Since BV is caused by bacteria, antibiotics are the most common course of treatment. If BV goes untreated, the disease can increase your risk of contracting other STDs.
Common antibiotics prescribed to treat BV include:
- Metronidazole (Flagyl, Metrogel-Vaginal). This may be an oral medication or a topical gel inserted into the vagina. Depending on how serious the infection is, any other medications you may be taking, and other factors, your doctor will prescribe treatment for three days to a couple weeks. While you take this prescription drug, it is important to avoid drinking alcohol and to follow your doctor’s instructions.
- Clindamycin (Cleocin, Clindesse). This is a cream inserted into the vagina. During treatment and for about three days after treatment, the cream can weaken latex condoms, so it is important to avoid sexual contact until your doctor says it is safe.
- Tinidazole (Tindamax). This is an oral antibiotic, which has similar risks of stomach upset or nausea as Flagyl. Follow your doctor’s instructions, and avoid drinking alcohol until treatment is complete.
- Chlamydia: This STD is caused by a small, parasitic bacterium. Both men and women can contract chlamydia, and most people who have this disease do not have symptoms. It is one of the most common STDs.While it is easily treated, it can cause pelvic inflammatory disease (PID) and difficulty getting pregnant for women. Men who contract chlamydia may have the infection spread to the epididymis (tube that carries sperm from the testicles), and it may cause chronic joint pain or infertility. Chlamydia is transmitted through oral, anal, or vaginal penetrative sex, through exposure to genital secretions. A male partner does not have to ejaculate to transmit chlamydia. Symptoms of chlamydia may include:
- Abnormal genital discharge.
- A burning sensation during urination.
- Pain or swelling in one or both testicles.
- Rectal pain, discharge, or bleeding (if contracted in the rectum).
Repeat infection of chlamydia is common, so if you contract this STD, it is important to avoid sexual contact until your course of treatment is complete and to inform your partner(s) of their potential exposure to this condition so they can also receive medical treatment.
Common antibiotics prescribed to treat chlamydia include:
- Azithromycin (Zithromax, Zmax). This is a relatively new antibiotic that inhibits bacterial protein synthesis. It is currently the leading prescription treatment for chlamydia, as it can be administered in a single dose, and it does not require multiple days of prescription medicine.
- Cefoxitin (Mefoxin). This medication is prescribed to treat bacteria like chlamydia that may be resistant to penicillin-based or cephalosporin-based antibiotics.
- Doxycycline (Adoxa, Doryx, Monodox, Avidoxy, Vibramycin). This is the second medication of choice to treat chlamydia, although the prescription requires one week of consistent oral medication. One week’s prescription of doxycycline drugs has been found to be as effective as one dose of azithromycin, and doxycycline costs less.
- Levofloxacin (Levaquin). This is not the prescription of choice, but it is an effective medication for drug-resistant chlamydia or repeated chlamydia infections.
- This medication works well for men who may have either genital or rectal chlamydia.
- Erythromycin (E.E.S., ERY-TAB, Erythrocin, EryPed, PCE). This antibiotic is used to treat pregnant women who have chlamydia. It may be used as a treatment for infants who have been exposed to chlamydia too.
- Gonorrhea: Like chlamydia, this STD is a fairly common bacterial STD, which most often affects people between 15 and 24 years old. The bacteria are transmitted through unprotected oral, vaginal, or anal penetration.If left untreated, gonorrhea can cause severe harm. Since the disease is very common, the bacteria are also increasingly becoming antibiotic resistant, so gonorrhea is becoming more difficult to treat. Both men and women can contract gonorrhea.Symptoms associated with gonorrhea include:
- Pain or burning when urinating.
- A white, yellow, or green discharge from the genitals or anus.
- Painful or swollen testicles.
- Bleeding between periods.
- Soreness in the rectum.
- Bleeding from the rectum.
- Painful bowel movements.
As new strains of antibiotic-resistant gonorrhea become more common, it is more important than ever to get regular STD testing if you are sexually active.
Uncomplicated gonorrhea is effectively treated with injection ceftriaxone in combination with oral Zithromax or Vibramycin. Factive oral (gemifloxacin) or injection gentamicin along with oral azithromycin (Zithromax) make up one of the most successful combinations of antibiotic treatments for gonorrhea. This combination can also be a better approach for those who are allergic to cephalosporin-based antibiotics.
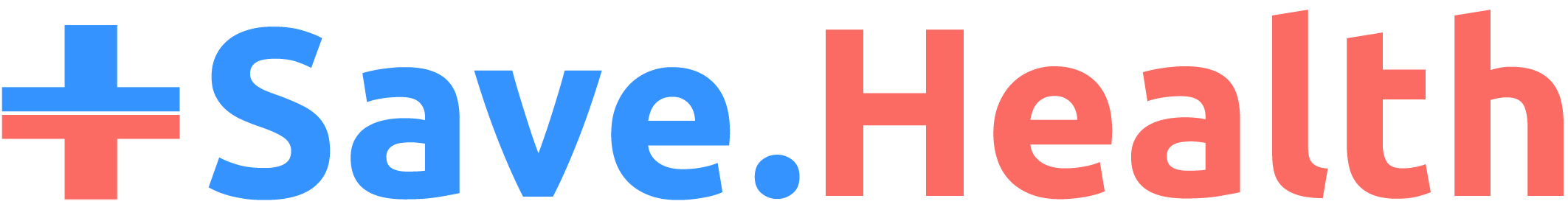
- Genital herpes: This STD is also herpes simplex 2, although increasingly herpes simplex 1 (oral herpes or cold sores) is transmitted through oral-genital contact.This is a common viral infection that may not display symptoms for several weeks or months after disease transmission. About one in every six people, between 14 and 49 years old, has genital herpes.The virus is transmitted through unprotected oral, anal, or vaginal penetration, and both men and women can contract this condition. Contact with a herpes sore, the saliva of someone who has oral herpes, genital discharge from someone who has genital herpes, or skin or blood contact with someone who has either disease can transmit herpes.Most people who have genital herpes do not have symptoms, or they will experience mild symptoms during an outbreak. Often, someone who has an outbreak of herpes can mistake the disease for a pimple or an ingrown hair. A herpes sore will look like a pimple or blister, and there will often be a cluster of them — on the lips, in the mouth, around the genitals, or around the rectum.The first outbreak is typically the most painful and noticeable. The blisters appear, itch or become painful, burst, and then take about a week or 10 days to heal. The first outbreak will also be accompanied by symptoms that feel like the flu, such as swollen glands, body aches, and fever.The herpes viruses are detectible in blood tests, so getting regular STD tests if you are sexually active, especially with multiple partners, is crucial. If you have an active outbreak of sores, your medical provider may also take a swab from the blisters.Herpes is a virus, so unlike bacterial diseases, there is no cure. Unlike some viruses, there are currently no effective vaccines against herpes. There are antiviral medications that can suppress viral load and reduce or shorten outbreak periods, which can lower the risk of transmitting the disease. Condoms are also very effective against herpes transmission, although they are not 100 percent effective.The three most common antiviral medications, which are daily oral pills, prescribed to treat herpes are:
These medications may suppress outbreaks completely, although they will not cure you of the herpes virus. HSV 1 and 2 are both very manageable chronic conditions, but you will need to follow your doctor’s instructions.
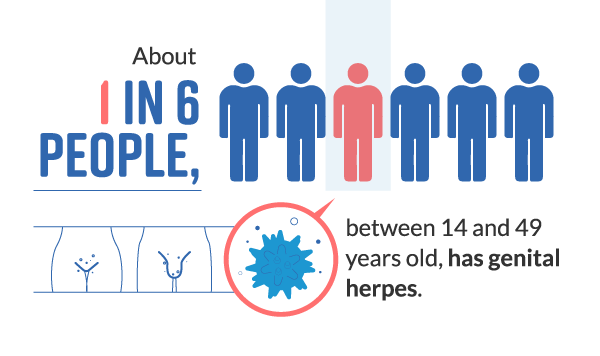
- HIV/AIDS: HIV is the acronym for human immunodeficiency virus, while AIDS is the acronym for acquired immunodeficiency syndrome.About 1.2 million people in the U.S. have HIV. There were an estimated 47,000 new HIV diagnoses in 2013 — 80 percent of these were men, and 20 percent were women. The number of people who have HIV in the U.S. is going up, but according to the CDC, this is because people who have HIV are living much longer than they did in previous decades. The rate of new HIV infections has remained about the same for the past several years.HIV is transmitted through contact with the semen, blood, vaginal secretions, rectal fluids, or breast milk of someone who is infected with either HIV or AIDS. Unprotected sexual contact and sharing needles for intravenous drug abuse are the two most common methods for HIV to be transmitted in the U.S.This virus attacks the body’s immune system, suppressing it and allowing other infections to become major problems.Currently, HIV tests are rapid and accurate, and treatment is effective. If you contract HIV, you will have this disease for the rest of your life, but it is very treatable.Untreated HIV may develop into AIDS. This process can take months, years, or even decades. There are three basic stages of HIV/AIDS infection.
- Stage 1, acute HIV infection: The disease takes hold about two to four weeks after infection, and it will cause flu-like symptoms, which may last longer than the average flu. Body aches, fever, and feeling nauseated are common immune system responses to any infection, which is why they present as initial symptoms of HIV.This initial stage is also the time during which many people are the most infectious. They have a lot of the virus in their bloodstream, but they are unaware they are infected.
- Stage 2, clinical latency: This period may also be called asymptomatic HIV or chronic HIV infection. The virus still reproduces in the body, but the immune system does not respond strongly to it. Most people do not experience symptoms or feel bad during this time, and the latency period may last for a decade or longer. The individual can still transmit HIV to others if they are not being treated.
- Acquired immunodeficiency syndrome (AIDS): This is the most serious stage of HIV infection. This stage occurs when untreated HIV severely damages the body’s immune system, which leads to increasing numbers of illnesses that are increasingly difficult to treat and can lead to death. People who have untreated AIDS have an average life expectancy of about three years.

People who are diagnosed with HIV will receive prescription medication treatment called antiretroviral therapy (ART). ART drugs reduce the viral load, or amount of active, reproducing virus in the blood and tissues of the body. This process is called viral suppression, and modern medicines in ART can reduce the viral load so much that HIV is virtually undetectable in blood tests.
Even if you have an undetectable viral load, it is important to continue taking your medications as directed and attending regular doctors’ visits as needed. Again, HIV is a chronic condition.
The following medications are approved by the United States Food and Drug Administration (FDA) to treat HIV:
- Nucleoside reverse transcriptase inhibitors (NRTIs): Ziagen, Viread, Retrovir, Epivir, Emtriva
- Non-nucleoside reverse transcriptase inhibitors (NNRITs): Viramune, Viramune XR, Sustiva, Pifeltro, Intelence, Edurant
- Protease inhibitors (PIs): Reyataz, Prezista, Norvir, Lexiva, Invirase, Aptivus
- Integrase inhibitors: Tivicay, Isentress, Isentress HD
- Fusion inhibitor: Fuzeon
- CCR5 antagonist: Selzentry
- Post-attachment inhibitor: Trogarzo
- Pharmacokinetic enhancer: Tybost
- Combination HIV medications: Atripla, Biktarvy, Cimduo, Combivir, Complera, Delstrigo, Descovy, Dovato, Epzicom, Evotaz, Genvoya, Juluca, Kaletra, Odefsey, Prezcobix, Stribild, Symfi, Symfi Lo, Symtuza, Triumeq, Trizivir, Truvada
Two additional, important advancements in the treatment of HIV include:
- PrEP. Prescribed under the brand name Truvada, PreP stands for pre-exposure prophylaxis. This medication is taken preventatively by someone who has been diagnosed with HIV. When taken consistently as prescribed, PrEP can reduce the risk of HIV transmission by 70 percent.
- PEP. This medication, called post-exposure prophylaxis, should be taken within 72 hours after being exposed or potentially exposed to HIV. It may cause nausea as a side effect in some people, but that is the only known side effect from this emergency medication. If you believe you have been exposed to HIV, your doctor will also test you for the virus six months after you have taken PEP.
- Human papillomavirus (HPV): This virus is the most commonly transmitted STD in the U.S. Both men and women can contract HPV, although women are most likely to experience symptoms, including abnormal cells on the cervix which, if untreated, can lead to cervical cancer. HPV has been correlated with oral, throat, penile, and rectal cancers, as well as genital warts.Young adults in their 20s are most likely to contract HPV, but anyone can contract it. Condoms are less effective against this virus than against any other STD. About 79 million Americans are estimated to have HPV.There are several strains of HPV, with some being higher risk than others. There is a three-dose HPV vaccine, which is effective for both men and women and recommended by many health care providers and agencies.There are currently no prescription treatments for HPV, unlike other STDs. Treatment involves removing genital warts or abnormal cells on the cervix.While even the high-risk strains of HPV tend to clear up on their own in two years or less, it is important to get regular medical checkups from a doctor to ensure the disease does not progress to a precancerous stage.
- Syphilis: This is a common bacterial STD spread through unprotected sex. While the disease is easily treated with antibiotics, it can be cause serious, permanent damage to the body if left untreated.The main symptoms of syphilis are sores (chancres) on the genitals. They are typically painless, but they will spread the infection to others who come in contact with them.Syphilis typically infects the genitals, but it can also infect the anus, lips, and mouth. If it is not treated early, syphilis can cause brain damage, paralysis, and blindness.Fortunately, regular STD testing if you are sexually active and some prescription antibiotics will catch and cure syphilis early. The preferred treatment for this disease at all stages is penicillin. A single injection can stop the disease from progressing, if you have been infected for less than one year. You may need additional doses if you have had syphilis for more than a year. You may also need different antibiotics if you are allergic to penicillin.
- Trichomoniasis: This is an increasingly common STD caused by a parasitic protozoan, Trichomonas vaginalis. Most people who develop “trich” do not know they have an STD because they are asymptomatic.Symptoms associated with trichomoniasis include:
- Itching or irritation inside the genitals.
- Burning after urination.
- Discharge from the genitals, especially if it is white, yellow, green, or has a fishy smell.
Both men and women can contract trich and spread it through unprotected sexual contact. Using condoms can reduce the risk of contracting trichomoniasis.
Treatment involves prescription antibiotics. Either metronidazole or tinidazole antibiotics are prescribed to treat this disease. There are few reports of resistant strains of trichomoniasis. It is important to complete your prescribed course of treatment.
Preventing STD Transmission
While STDs have a variety of approaches to treatment, there are a few standard methods to prevent disease transmission.
Here are the best methods for preventing contraction of an STD:
- Abstinence: The only way to be sure you will not contract an STD is to avoid sexual contact.
- Reduced number of sexual partners: Having more sexual partners increases your risk of exposure to an STD. Limiting the number of people you have sex with can reduce your exposure and therefore your risk.
- Mutual monogamy: If you have a consistent partner, agree to avoid sexual contact with others and only have sex with each other.
- Regular testing: Regardless of how many partners you have, getting regular STD tests can help you know if you have contracted an STD, so you can get prompt treatment. Ask your doctor about what testing schedule suits your needs best. Once a year or every six months is a common timeframe, depending on your number of sexual partners.
- Vaccination: There are vaccines to prevent or reduce the risk of many STDs, including hepatitis and HPV.
- Condoms: Condoms reduce the risk of both STD transmission and pregnancy. While they are not 100 percent effective in every case, latex condoms provide the most protection against all STDs if you are sexually active.
Frequently Asked Questions
What are STDs?
The acronym STD stands for sexually transmitted disease. These are also often referred to as sexually transmitted infections (STIs).
These diseases are transmitted between people through unprotected sexual contact — typically, oral, vaginal, or anal penetration. These diseases can be caused by parasites, viruses, bacteria, fungi, or protozoans.
How are STDs spread?
STDs are spread through fluid or mucous membrane contact, which includes semen, vaginal secretions, rectal fluids, saliva, and blood. Contact with sores, pustules, or blisters caused by the STD may also lead to transmission.
Can STDs be prevented?
Yes. Abstinence is the most effective way to ensure you do not contract an STD. Other methods include remaining monogamous with one partner, limiting how many sexual partners you have, and receiving preventative medical treatment like vaccines.
Getting regular STD tests and using condoms are the most effective ways for sexually active people to manage their sexual health, by knowing their STD status and reducing their risk of transmission.
What are the most common STDs in the United States?
- Chlamydia
- Gonorrhea
- Genital herpes
- Human papillomavirus (HPV)
- HIV/AIDS
- Syphilis
- Trichomoniasis
There are other STDs, and other diseases can be transmitted through unprotected sexual contact. Report any symptoms or any unprotected sexual contact to a medical professional if you are concerned about disease exposure.
What medications are used to treat STDs?
Most bacterial STDs are curable through a regular course of antibiotics; however, some diseases, like late-stage syphilis or antibiotic-resistant gonorrhea, can be difficult to treat. Viral infections, like HIV, herpes, and HPV, are not curable, but they are very treatable.
References
CDC Fact Sheet: Information for Teens and Young Adults: Staying Healthy and Preventing STDs. (May 22, 2104). Centers for Disease Control and Prevention (CDC).
Bacterial Vaginosis – CDC Fact Sheet. (February 8, 2017). Centers for Disease Control and Prevention (CDC).
Bacterial Vaginosis: Diagnosis and Treatment. (July 29, 2017). Mayo Clinic.
Chlamydia – CDC Fact Sheet. (January 23, 2014). Centers for Disease Control and Prevention (CDC).
How Do I Get Treated for Chlamydia? Planned Parenthood.
Chlamydia (Chlamydial Genitourinary Infections) Medications. (September 25, 2018). Medscape.
Gonorrhea – CDC Fact Sheet. (January 29, 2014). Centers for Disease Control and Prevention (CDC).
Gonorrhea: Diagnosis and Treatment. (February 6, 2018). Mayo Clinic.
Genital Herpes – CDC Fact Sheet. (August 28, 2017). Centers for Disease Control and Prevention (CDC).
Genital Herpes Treatment and Care. (December 9, 2016). Centers for Disease Control and Prevention (CDC).
Genital Herpes Treatment – Antivirals and Safer Sex. (March 28, 2018). Everyday Health.
General HIV Information: HIV Risk Reduction Tool. Centers for Disease Control and Prevention (CDC).
HIV in the United States. Centers for Disease Control and Prevention (CDC).
Stages of HIV Infection. Centers for Disease Control and Prevention (CDC).
Antiretroviral Therapy (ART) for Treating HIV. Centers for Disease Control and Prevention (CDC).
FDA-Approved HIV Medications. (April 12, 2019). AIDS Info, National Institutes of Health (NIH).
Pre-Exposure Prophylaxis (PrEP) for Preventing HIV. Centers for Disease Control and Prevention (CDC).
Post-Exposure Prophylaxis (PEP) for Preventing HIV After Exposure. Centers for Disease Control and Prevention (CDC).
Genital HPV Infection – CDC Fact Sheet. (November 16, 2017). Centers for Disease Control and Prevention (CDC).
Syphilis. Planned Parenthood.
Syphilis: Diagnosis and Treatment. (January 16, 2019). Mayo Clinic.
Trichomoniasis – CDC Fact Sheet. (January 31, 2017). Centers for Disease Control and Prevention (CDC).
Trichomoniasis Treatment and Care. (January 4, 2017). Centers for Disease Control and Prevention (CDC).
How You Can Prevent Sexually Transmitted Diseases. (January 21, 2016). Centers for Disease Control and Prevention (CDC).