Tick bites are very common in the United States. In most cases, they cause very little distress. (Learn More, What Are Ticks?)
Some ticks carry bacteria, viruses, and parasites, which they pass on to human hosts in a bite. These can cause moderate to severe diseases, which require medical treatment. (Learn More, What Is the Treatment for Tick-Borne Diseases?)
Timing is very important. You should go to a doctor as soon as you are bitten. This gives you the best chance of ensuring that the bacteria, virus, or parasite is addressed before it causes long-lasting damage.
For Lyme disease, treatment usually involves antibiotic medications and acetaminophen for pain and fever. Fluids and rest are recommended to recover strength. (Learn More, Lyme Disease)
Some tick-borne diseases, like Colorado tick fever, have no known treatment, meaning that speedy medical intervention becomes all the more vital. (Learn More, Colorado Tick Fever)
What Are Ticks?
Healthline explains that ticks are very common in the United States, found in grass, trees, shrubs, and even just piles of leaves. They seek out people and animals, including pets, easily moving from one to the other.
Ticks like to make themselves comfortable in warm, damp areas of the body, such as the armpits, the groin, or anywhere where hair is thick. When they feel comfortable, they bite into the skin and begin drawing blood.
More often than not, tick bites are harmless, and they do not cause any noticeable symptoms. In some cases, ticks can cause allergic reactions in people. Some ticks are capable of passing on diseases from one host to another, through the process of the bite. These diseases can be dangerous and even fatal if they are not treated in time.
Unique among insects that bite, ticks will stay on the body even after they bite. It can take a full 10 days of drawing blood until the tick gets so engorged on blood that it falls off.
In most cases, tick bites are harmless and might not even be noticed. However, someone who is allergic to a tick bite will note pain or swelling at the bite site, a rash, blisters, and, in cases of a severe allergy, difficulty breathing.
Ticks and Diseases
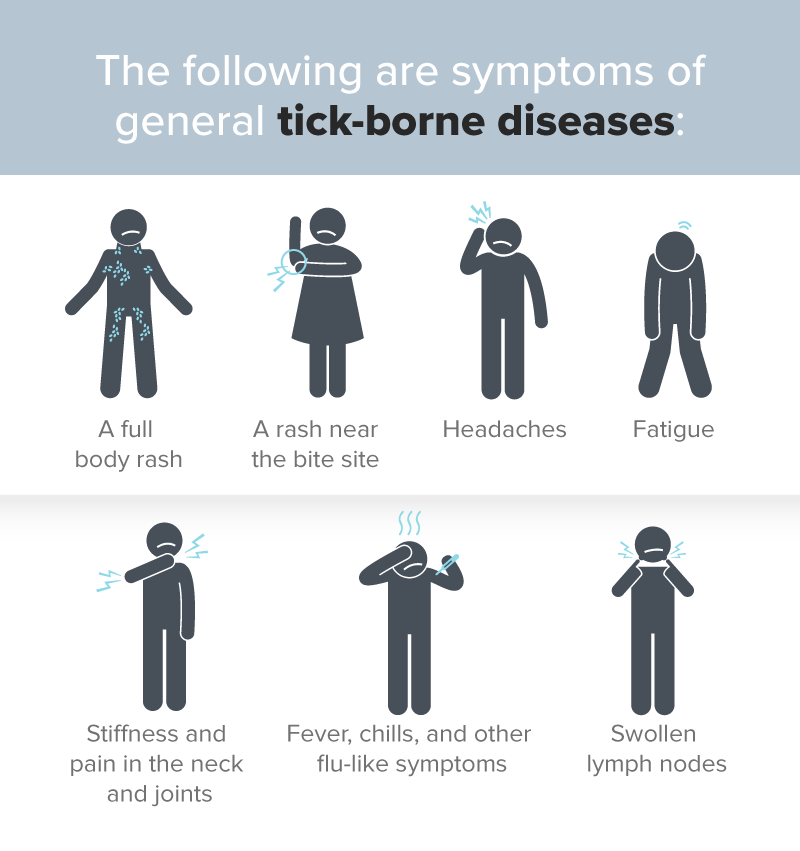
Some ticks carry bacteria, viruses, or parasites, all of which can cause disease and are passed on to the host when the tick bites. The diseases can cause severe symptoms, and they will start to show within days or weeks of the bite.
Tick Bites and Other Problems
Tick bites can lead to other problems, even if the symptoms of those other problems have not yet presented themselves. In places where Lyme disease is common, for instance, doctors might want to be proactive in responding to the risk that a patient has contracted Lyme disease from a tick bite. They might start treatment for Lyme disease after the patient reports the tick bite even if none of the symptoms of Lyme disease are present.
If there is a danger that a tick bite might lead to Rocky Mountain spotted fever, another tick-borne disease, the presence of a tick bite might be enough to start treatment.
Any symptoms following the tick bite — rash, joint pain, fever, unexplained changes to health and wellbeing — should prompt medical care, out of an abundance of caution. Tick-borne diseases can easily lead to medical emergencies.
What Is The Treatment for Tick-borne Diseases?
Treatment starts with the tick bite itself. The first and most important step is to remove the tick. A set of tweezers should be enough to pull the tick straight up from the skin’s surface. Do not bend or twist the tick, as this may not properly remove it from the site. Make sure that no part of the tick’s head or mouth is left in the bite (even if the body itself is removed).
Don’t discard the tick’s body. Place it in a sealed container, so doctors will be able to tell what kind of tick it is. They may test it to see what bacteria, virus, or parasite it may or may not have passed on to you.
Clean the bite site with soap and water. Then, see a doctor as soon as possible to determine what treatment is necessary.
Preventing tick bites is also a form of treating tick-borne diseases. When walking in the woods or in grassy areas where ticks are often found, wear a long-sleeved shirt and pants (not shorts). Walk in the center of trails, and do not go off the path.
Buy a good tick repellant, and make sure to shower thoroughly within two hours of being outdoors. Check your armpits, groin, hair, and behind your knees for any unexplained bites, scratches, redness, or rashes.
It generally takes a little over 24 hours of a tick drawing blood to pass on a disease to its host. The sooner you identify a tick bite, remove the tick, and get treatment for a possible tick-borne disease, the better.
Examples of Tick-Borne Diseases
But what exactly are tick-borne diseases? The Centers for Disease Control and Prevention warns that a tick can pick up a bacteria, virus, or parasite from one host and then pass it on to another.
The following are some well-known tick-borne diseases in the United States:
- Tularemia
- Tick-borne relapsing fever
- Southern tick-associated rash illness
- Anaplasmosis
- Rocky Mountain spotted fever
- Lyme disease
- Ehrlichiosis
- Babesiosis
Other tick-borne diseases are Q fever, Colorado tick fever, and Powassan encephalitis.
Lyme Disease
 People who have outdoor jobs are at the highest risk of picking up a tick-borne disease, especially if they work at a site where ticks are found. Such sites feature woods, bushes, high grass, or leaf litter. In regions with warmer weather, ticks may be active all year.
People who have outdoor jobs are at the highest risk of picking up a tick-borne disease, especially if they work at a site where ticks are found. Such sites feature woods, bushes, high grass, or leaf litter. In regions with warmer weather, ticks may be active all year.
Lyme disease is caused by the Borrelia burgdorferi bacteria, which humans get when they are bitten by a black-legged or deer tick that is carrying the bacteria. Symptoms can show in as little as three days or as many as 30. It is not unheard of for some patients to only show their first symptoms months after the first bite.
WebMD writes that ticks have to be attached to a human host for 36 to 48 hours in order for the bacteria to pass over. If the ticks are removed within 48 hours, the chance of infection drops, but patients should still get examined.
Mayo Clinic explains that antibiotics are used in the treatment of Lyme disease. Again, the sooner the regimen starts, the better.
Treating Lyme Disease
Oral antibiotics are normally issued for Lyme disease that is still in its early stages. Adults and children older than the age of 8 will receive doxycycline. Younger children and pregnant or breastfeeding women will receive amoxicillin or cefuroxime. A three-week course will suffice, but some patients may be healed by the second week.
In middle- or late-stage Lyme disease, where the central nervous system has become compromised by the spread of bacteria, a patient might have to be put on an intravenous antibiotic drip for upward of a month. This is the most effective way of eliminating the infection. This form of treatment means that the disease has had a lot of time to wreak havoc with the body, so recovery from symptoms could take months.
Intravenous antibiotic treatment for Lyme disease and other tick-borne diseases comes with its own side effects, such as:
- A reduced white blood cell count.
- Potentially severe diarrhea.
- Infection with other antibiotic-resistant bacteria, parasites, or viruses that may be unrelated to Lyme disease.
The Reumatologia journal writes that even after receiving treatment for Lyme disease, a small number of patients (around 10 percent) will still have some symptoms, like fatigue and pain in the muscles and joints. This is a condition known as post-Lyme disease syndrome, which is still poorly understood. Further antibiotic treatment will not address it.
Rocky Mountain Spotted Fever
Rocky Mountain spotted fever was first identified in the Rocky Mountains as a tick-borne disease, but it is now more commonly found in the southeastern United States. Cases have also been documented in South America, Central America, Mexico, and Canada.
A few days after the bite, a red, non-itchy rash will appear on the ankles and wrists. It spreads onto the palms of the hands and soles of the feet, and up to the arms and legs to the torso. Some people who are infected with Rocky Mountain spotted fever from a tick bite don’t ever develop a rash, which is an impediment to getting timely treatment.
Symptoms of Rocky Mountain spotted fever include a painful headache and very high fever, but these may not show for up to two weeks. The first signs of Rocky Mountain spotted fever are very ambiguous, and they are often mistaken for other conditions. This might lead to a delay in a patient seeking appropriate treatment, which can end up being very damaging for their health.
Treating Rocky Mountain Spotted Fever
As with Lyme disease, Rocky Mountain spotted fever can be treated with the antibiotic doxycycline. This medication is usually administered to children and adults. Pregnant or breastfeeding women, as well as very young children and certain other patients, might receive chloramphenicol instead.
The Centers for Disease Control and Prevention recommends that patients who are bitten by a tick get tested for Rocky Mountain spotted fever immediately, especially in places where cases of this particular tick-borne disease are common. A delay in treating the infection can make the disease very hard to successfully treat, and this can be very painful for the patient. In an ideal circumstance, treatment will begin within five days of the tick bite, if not sooner.
A delay might require the use of intravenous antibiotics and a lengthy hospital stay.
Colorado Tick Fever
Unlike most other forms of tick-borne diseases, Colorado tick fever does not have, or require, a specific treatment. The Medical Clinics of North America journal calls Colorado tick fever a “self-limited disease,” meaning that it usually resolves itself without the need for medical intervention.
When the symptoms of Colorado tick fever first develop, they normally fade away on their own within 10 days. Patients may take acetaminophen and other pain relievers to soothe the fever and muscle pain. A period of rest and taking in more fluids will also be helpful.
The only time Colorado tick fever can be a problem is if other bacterial infections were also contracted at the time of the initial tick bite or if the flu and discomfort of the fever exacerbate other health conditions. Notwithstanding that Colorado tick fever is an unusually mild tick-borne disease, it is still a good idea to get checked for other conditions.
Powassan Virus
In most cases of tick-borne diseases, the tick needs to be attached to the skin for around 36 hours in order for the bacteria to make its way into the host’s bloodstream. However, in the case of Powassan virus, studies have found that it takes only 15 minutes for humans to become infected.
The Powassan virus is still relatively rare in the spectrum of tick-borne illnesses. It was only in 2008 that the first recognized cases were reported in the United States. As recently as May 2019, only 33 patients have been diagnosed with it. Nonetheless, Powassan virus is serious enough that it has become part of the general conversation on treating diseases passed on by ticks.
Symptoms of Powassan virus are all over the map. Some patients will experience only minor distress, while others can become seriously sick to the point of death. It can take anywhere from a week to a month from the time the tick bites to the time the first symptoms start to show themselves.
Symptoms of Powassan Virus
Powassan virus (named after a town in Ontario, where it was implicated in the death of a young boy) can target the central nervous system, leading to meningitis (swelling of the membranes around the brain and spinal cord) and encephalitis (swelling of the brain itself). More general symptoms include the following:
- Headache
- Vomiting
- Fever
- Weakness and fatigue
- Mental disorientation
- Speech difficulties
- Seizures
As many as half the people who get the Powassan virus from a tick bite will go on to develop permanent symptoms, like recurring headaches, muscle problems, and memory problems. Ten percent of cases of Powassan virus are fatal.
Dealing With Powassan Virus
Because Powassan virus is so rare, there is no established treatment for it. The only care that can be provided is supportive care, with the hope that it is administered quickly enough to stop the virus before it spreads to the brain and central nervous system. A diagnosis of Powassan virus, based on blood tests and observation of symptoms, will likely result in long-term hospitalization, with breathing support, intravenous fluids, and drugs to reduce meningitis and encephalitis.
Troublingly, a tick that passes on the Powassan virus can also have bacteria for another related disease, like Lyme disease. A patient being treated for one tick-borne condition should be checked for another, like Powassan virus.
A Growing Need for Treatment
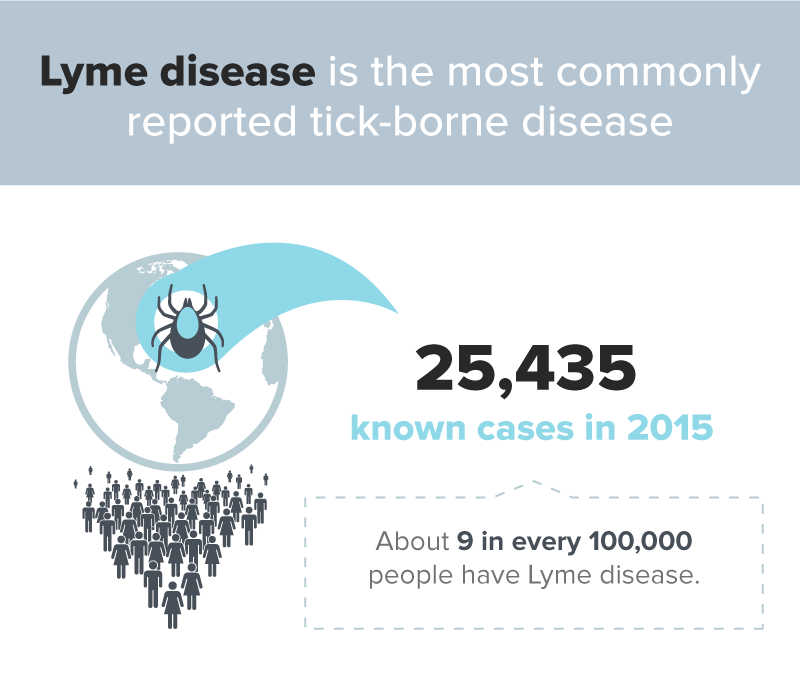
Treating tick-borne diseases has become increasingly important because the number of reported tick-borne diseases are on the rise.
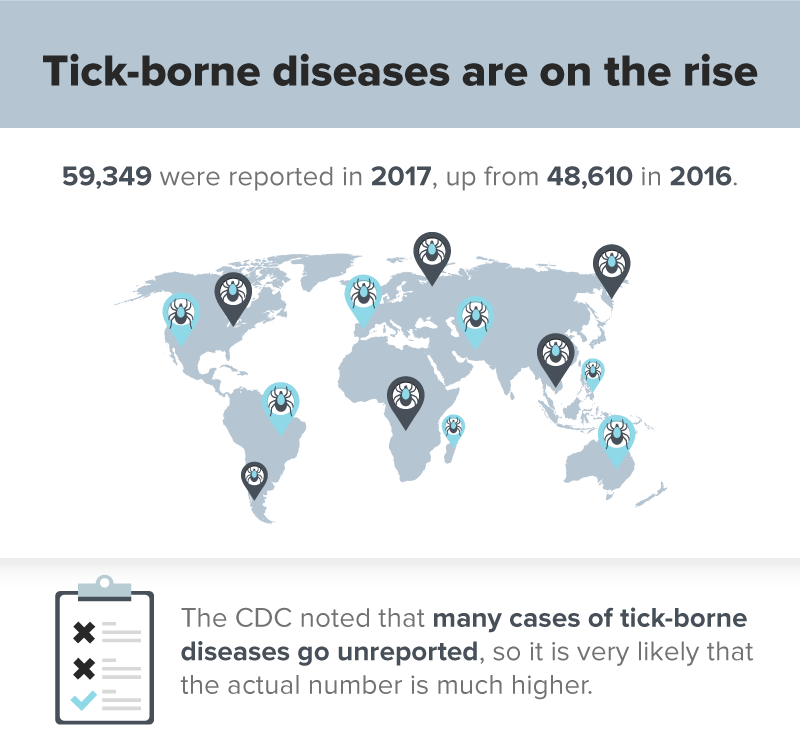
The reason for this is not known, although scientists point out that there are many disparate factors that affect the yearly tick populations (rising temperatures and humidity, and the movements of host animals like mice and deer expanding the range of ticks). With these, the likelihood of certain forms of tick-borne illnesses spreading increases. JAMA notes that there have even been concerns of “new diseases” emerging through ticks.
On the human side, availability and access to health care, as well as education about tick-borne diseases, can also affect the reporting of those conditions.
Regardless of causes, the CDC warns that the United States is not ready to counter the threat of rising tick-borne diseases, which will make them that much harder to treat.
References
Tick Bites: Symptoms and Treatments. (May 2017). Healthline.
How to Remove a Tick. (October 2018). WebMD.
Tick-Borne Diseases. (September 2011). Centers for Disease Control and Prevention.
Lyme Disease: What to Know in 2018. (August 2018). WebMD.
Lyme Disease. (July 2019). Mayo Clinic.
Post-Lyme Disease Syndrome. (2015). Reumatologia.
Rocky Mountain Spotted Fever. (October 2017). Mayo Clinic.
Everything You Need to Know About Rocky Mountain Spotted Fever. (April 2017). Healthline.
Signs and Symptoms. (February 2019). Centers for Disease Control and Prevention.
Colorado Tick Fever. (January 2016). Healthline.
Colorado Tick Fever. (March 2002). The Medical Clinics of North America.
Colorado Tick Fever: Symptoms, Treatment, And Prevention. (July 2017). Medical News Today.
Powassan Virus — A New Re-emerging Tick-Borne Disease. (December 2017). Frontiers in Public Health.
What Is Powassan Virus? This Tick-Borne Illness Can Cause Fatal Swelling of the Brain. (May 2019). Health.
What Is Powassan Virus? Symptoms and Treatment of the Tick-borne Disease. (August 2019). Today.
2 Cases of Tick Borne Powassan Virus Confirmed in Northern New Jersey. (June 2019). CNN.
Man “Lucky” to Be Alive After Getting Powassan Virus From Tick Bite. (June 2017). CBS News.
Record Number of Tick Borne Diseases Reported in U.S. in 2017. (November 2018). Centers for Disease Control and Prevention.
Tick Borne Diseases Increasing. (2019). JAMA.