When it comes to staying healthy in 2022, there are a lot of things you can do. A healthy lifestyle is the basis for good health, and this includes regular visits to a doctor for preventative care.
Every flu season, the question over whether to take care of the bug at home or go to a doctor is on the minds of millions of people. (Learn More) Despite much misinformation to the contrary, getting vaccinated is still the best line of defense from communicable diseases. (Learn More)
Home remedies for sickness can offer some benefits, but they are limited in what they can do. (Learn More) Parents with young children can try some simple solutions when their kids get sick, but the appearance of any painful or severe symptoms is a good reason for a doctor’s visit (Learn More)
We have a lot of information about how to stay healthy in 2022, but there is also a fair share of misinformation and threats to public and personal health out there. This guide to health will cover some of the standard approaches on how to look after yourself and also address some of the contemporary problems with staying healthy.
Should I See a Doctor for the Flu?
The flu is usually on its way out by May, but in April 2019, the Centers for Disease Control and Prevention warned that the three types of influenza virus still do the rounds, and people getting sick over the summer is not unheard of. But how do you know when you should see a doctor for a cold or flu?
WebMD answers this by advising people to “take stock of their symptoms,” to know when they’ve got just a simple seasonal bug and when it’s a more serious problem.
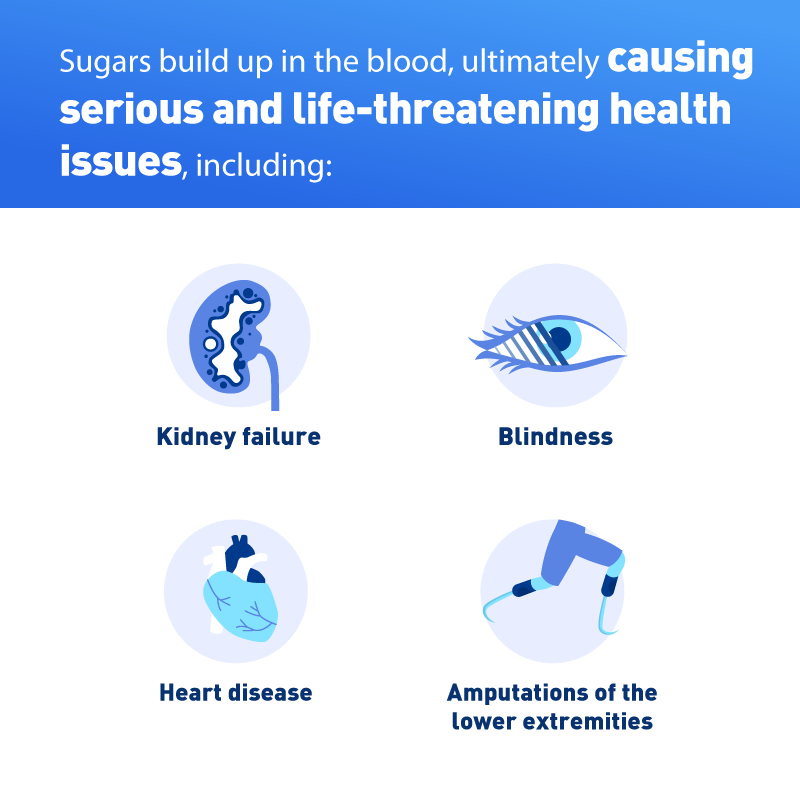
The first serious symptom is chest pain or trouble breathing. A regular cold (or even the flu) shouldn’t make it difficult to breathe or cause pain in the chest. This can be a sign of pneumonia, heart disease, or asthma.
If the fever persists for more than four days, this might be an indication that the flu has exacerbated another infection. Related to this is the danger of vomiting or diarrhea. If your body can’t keep in any of the food or drink you take in whilst you are sick, this is a serious warning sign of a larger problem than a regular flu. You should go to an emergency room or urgent care clinic immediately.
Coughs and Headaches
Similarly, a cough that doesn’t go away could easily be postnasal drip (mucus that trickles from the nasal cavity down to the throat), and it is treated with simple antihistamines. However, persistent coughing could be a sign of asthma or gastroesophageal reflux disease, or GERD. A cough that doesn’t seem to go away, even after a week of rest and treatment, should be looked at by a doctor.
Whooping cough is a serious problem. Even if you’ve been vaccinated for it, CNN warned in June 2019 that the vaccine becomes less effective over time. If your cough continues for weeks, then a doctor’s visit is definitely worth it.
Likewise, congestion and headache for the flu is not unexpected, but there is the possibility of developing a sinus infection. Over-the-counter cold medicine should help clear the blocked nose (or make it more bearable), but if the headache and stuffiness remain, a doctor should take a look at it.
Experiencing some discomfort when you swallow is a common symptom of a sore throat, but it should not cause severe pain. If trying to swallow becomes so painful that consuming any liquid or food becomes prohibitively difficult, this is a sign of another infection. It brings a risk of malnutrition at a time when your body really needs all the help it can get. Medical News Today writes that unusually and severely painful swallowing is a good reason to visit a doctor, even if everything else looks like a normal bug.
Getting Vaccinated
Getting vaccinated against the flu is part of a much larger conversation about vaccinating against communicable diseases in 2022.
NPR writes of how previously controlled diseases like measles are on the rise again, with a record 700 cases being reported in America in 2022. It’s the highest number since the disease was first eliminated in 2000. More than three states have experienced outbreaks, with the state of Washington declaring a state of emergency in January 2019 over the epidemic.
The current vaccine recommended by the CDC is the MMR vaccine, for measles, mumps, and rubella. It is recommended that children get two doses — the first between the ages of 12 to 15 months, and second between the ages of 4 to 6 years old.
Communicable diseases like the flu and measles rank among the 10 threats to global health in 2022, outlined by the World Health Organization. One of the drivers of these threats is what WHO calls “vaccine hesitancy,” which it defines as the reluctant or outright refusal to vaccinate, even though vaccines are available. This is a problem because not vaccinating can reverse the progress made in controlling the spread of diseases that can be prevented by children and adults having regular vaccinations.
Vaccine hesitancy has seen measles increase by 30 percent around the world. Not all cases are due to refusal to vaccinate. In many cases, this is because patients simply don’t have access to safe and reliable health care for economic or cultural reasons. But regardless of the reasons, measles is experiencing a resurgence globally and in the United States as well.
The Best Protection
The point is contested by Vox, which writes that as the measles epidemic is likely to spread across the United States for the rest of 2019, “there is no disagreement that vaccine refusal is the cause of outbreaks.” As many as 70 percent of the reported cases of measles were in people who were not vaccinated, and 88 percent of the cases were located in communities with below-average rates of immunization.
Regardless of the controversy, the Food & Drug Administration confirmed in May 2019 that “vaccination is the best protection against measles.”
Home Remedies vs. Doctor Visits
It’s not easy paying for hospital visits. Many people wonder when they can take care of themselves and their loved ones at home, and when they should see a doctor.
The State Press out of Arizona State University explains that while home remedies can be “a very effective and cheap way to cure myriads of problems,” there is some trial and error involved. Some home remedies derive their effectiveness from the medically beneficial properties in their ingredients and (to a varying degree) the strong belief that people have that the remedies offer as much of a cure as pharmaceutical products.
There are psychological and physiological circumstances of a person taking the home remedy that can go a long way in offering relief from their condition or the remedy having no effect. The same principle applies to prescribed medication.
So when do home remedies not cut it anymore? A nursing student at ASU said that if the remedies are actively proving unhelpful or if they are interfering with the patient’s well-being, the time has come to go to a pharmacy for some over-the-counter medicine or to consult a doctor if there is a concern that a bigger problem might be at play. The rule of thumb is that minor ailments can be quickly and affordably treated at home (maybe with some assistance from simple medication that doesn’t require a prescription), but if the illness interferes with the patient’s daily life or causes undue stress and grief, then a doctor’s visit is imperative.
“Certain home remedies may work for you,” says The State Press, but they can quickly fall well short of the potency and necessity of prescribed medication.
When Should My Child See a Doctor?
Parents of young children will have many questions about their child’s health care. For example, how often should you take your child to the doctor? Most pediatricians will recommend a yearly visit to evaluate key markers of your child’s health and growth. Such markers include:
- Development, including speech, motor skills (including precise and general skills), and social interaction, especially in their developing years. Any delays can be quickly spotted, and appropriate therapies applied.
- Nutrition and exercise, to make sure the child is eating properly (specifically, getting the proper amount of food and vegetables) and staying active.
- A routine physical exam, to help a doctor detect any changes that the parents may have missed.
Answering questions is a huge part of making sure your child stays healthy. A doctor’s appointment is the perfect time to talk about any health issues affecting your child and your family, and you can get advice and insight from a medical professional. It helps to make a list of questions before the appointment.
If your child has a chronic illness, a regular pediatrician visit will help them stay healthy and out of the hospital. The yearly visit will also allow parents to get refills for their child’s medications.
Lastly, regular visits help parents and children develop a relationship with their doctor. The pediatrician needs to know the family, so they have a good foundation to recognize any changes (positive or negative) that occur.
Pediatricians who don’t see patients and parents regularly will miss vital signs about a child’s health because there is no continuity of care present in the arrangement. Knowing your doctor builds a vital foundation of trust and familiarity, which will greatly help you, your child, and your family stay healthy.
Home Care for Your Child
On a day-to-day basis, many minor concerns and ailments can be treated at home. Even very young children have immune systems that can take care of basic conditions (although the child will still be sick and need care). Infrequent coughs, for example, can be easily treated with a cool-mist humidifier and lots of fluids. Children should get plenty of rest and home-based remedies, like chicken soup.
During flu season, it is advisable to keep your child at home if:
- They have a fever of over 101 degrees Fahrenheit.
- They find it difficult to concentrate on schoolwork or participate in activities.
Recuperating at home is often the best way to recover from seasonal ailments.
The American Academy of Pediatrics strongly advises against giving children ages 6 and under over-the-counter cough medication. Check with your doctor before giving your children any pharmaceutical products, no matter how benign they may seem.
If what started as a simple cough leads to fever-like symptoms, or if the cough itself is frequent, painful and dry, then it is best seen by a doctor. Such symptoms could be a symptom of whooping cough or a respiratory problem. Other serious developments — like vomiting and diarrhea, blood in stool or vomit, fatigue, exposure to a contagious illness, excessive fatigue, and dehydration — are reasons enough to go to a hospital.
As a rule of thumb, when it comes to making the decision about whether or not to take your young child to the emergency room, it is advisable to err on the side of caution. Any problems you notice in children under 4 months of age should be immediately examined by a doctor.
Staying Healthy in 2022
Medical Economics writes of other ways to stay healthy in 2019, such as the continued and improving integration of technology and medicine. Telehealth and telemedicine solutions will offer “an infinite number of possibilities for connecting patients and clinicians remotely.”

With nothing more than a smartphone and an internet connection, doctors can provide virtual, cost-effective visits to patients who cannot leave their homes or who live too far away to make appointments. The right kind of software can allow doctors to prescribe certain medications, and patients can pick up those medications from participating pharmacies.
Telemedicine also means that doctors will be able to provide more face-to-face care with local and able patients while still being able to track the progress of patients who live much farther away. The technology also allows for more continuity of care, suggesting that 2019 will be a year of more personal health care access, for both patients and doctors alike.
References
Flu Season Isn’t Over Yet — and More Serious Strains Are on the Rise, CDC Says. (April 2019). TIME.
When Should I See a Doctor For a Cold Or The Flu? (November 2018). WebMD.
Whooping Cough Vaccine Becomes Less Effective Over Time, Study Says. (June 2019). CNN.
How to Deal With a Sore Throat. (February 2019). Medical News Today.
Measles Shots Aren’t Just for Kids: Many Adults Could Use a Booster Too. (April 2019). NPR.
Washington State Officials Declare State of Emergency as Measles Outbreak Continues. (January 2019). NPR.
Ten Threats to Global Health in 2019. World Health Organization.
I’ve Talked to Dozens of Parents About Why They Don’t Vaccinate. Here’s What They Told Me.” (June 2019). Vox.
Vaccination Is the Best Protection Against Measles. (May 2019). U.S. Food & Drug Administration.
Using Home Remedies Versus Prescription and Over-the-counter Medication.” (February 2018). The State Press.
Just Because a Natural Remedy ‘Works’ for You Doesn’t Mean It Works. (June 2017). Self.
Ask the Pediatrician: How Often Should I Take My Child to the Doctor? (March 2017). Mount Nittany Health.
When to Call the Pediatrician. (July 2017). WebMD.
The Importance of Having a Relationship With Your Child’s Pediatrician. (July 2018). Nationwide Children’s.
Does Chicken Soup Really Help Fight a Cold? (March 2018). CNN.
Cough and Cold Medicine — Not for Children. American Academy of Pediatrics.
When to Take Your Sick Child to the Doctor. (March 2019). Verywell Health.
Top 4 Healthcare Trends for 2019. (March 2019). Medical Economics.