Getting a Prescription Without a Doctor (A Guide)
About half of all Americans take one prescription medication each and every day. Short doctor visits, savvy pill marketing, and habit convince us that every doctor's appointment should end in a prescription. (Learn more) But what happens when you don't have a doctor's appointment, and you need a medication solution? Federal and state laws can keep you from getting some kinds of medications without an in-person doctor's visit. Proposed legislation may change that soon, but for now, you will need to make an in-person visit to get some kinds of medications. (Learn more) But there are workarounds to these seemingly firm rules. You could have a virtual visit with a doctor and get some prescriptions filled, or you could visit some types of pharmacies to get help. Some doctors will even help you get the medications you need with a phone call rather than a visit. (Learn more) To ensure you don't get stuck when you're sick, make a connection with a telehealth provider now and build a relationship with your doctor. You'll have several options open to help you get the solutions you need, even without an appointment. (Learn more)
Medication Use Is Rampant
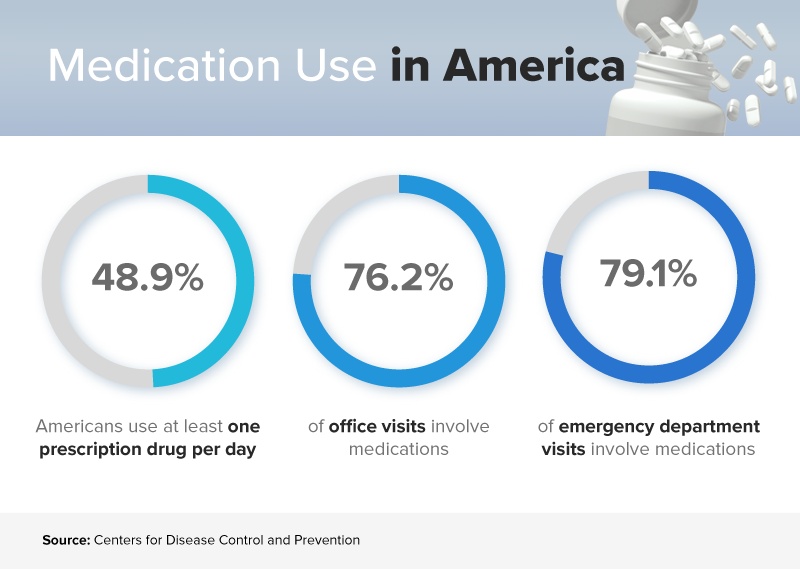
Your body is remarkable, and it's capable of addressing all types of illnesses without any help from a doctor at all. But some illnesses require medication management, and some issues need urgent pill help to resolve. Our doctors — and our preferences — also play a role in how many medications flood the marketplace and how many of us take them. Consider these three statistics from the Centers for Disease Control and Prevention:
Percentage of Americans using at least one prescription drug per day: 48.9
Percentage of office visits that involve medications: 76.2
Percentage of emergency department visits that involve medications: 79.
Why do we use so many medications? And why do we think they're necessary? Experts have a few ideas. They blame the trend on:
Short office visits. Primary care visits are often about 15 minutes long, says
Kaiser Health News, and those mini-appointments up the chances that you'll leave the office with a prescription. Doctors don't have time to talk to you about changing your lifestyle, eating habits, or exercise routines. They hand out pills and potions instead.
Marketing tactics. It's legal for pharmaceutical companies to pop ads in television programs, on websites, or in magazines. Read them, and you're encouraged to "talk to your doctor" about whether the drug is right for you. Messages like this inspire you to think of drugs as the solution to any health care problem you might have, even if that's not true.
Patient preference. National Public Radio reports that people give their doctors high customer satisfaction scores when they get drugs — even if the medications can't treat them. People who get antibiotics for colds, for example, tend to be happier than those who don't get a prescription.
It's not always wrong to get a medication prescription. If you have diabetes, heart disease, depression, or another chronic health condition, your prescription could mean the difference between being healthy and resting in the hospital. And you might not know if you even need medication unless you talk to a doctor first. It's that thinking that has prompted legislative work.
Federal Laws Make Doctors Get Involved
Harried doctors under pressure are likely to give their patients any medication they've asked for. But lawmakers want doctors to make decisions about drug solutions, and they've written laws that force doctors to do just that. In 2008, after the death of a young man who overdosed on painkillers he bought online, Congress passed an act in his name. The Ryan Haight Act prohibits doctors from prescribing controlled substances online without a valid prescription. And according to the law, that prescription must be:
Issued for a legitimate, specific purpose.
Issued once a doctor has conducted at least one in-person evaluation.
As Epstein Becker Green points out, this law was designed to keep people from dying due to prescription opioids. But there are all sorts of medications officials consider controlled substances, including:
Robitussin AC or other cough medications that include codeine.
Adderall, Dexedrine, and other prescription stimulant drugs.
Xanax, Klonopin, or other benzodiazepine medications to treat anxiety.
Suboxone or other buprenorphine drugs to treat addiction.
Depo-Testosterone and other anabolic steroids.
According to Modern Healthcare, there are at least eight states that allow doctors to hand out controlled medications after virtual office visits conducted via phone or video chat. These telemedicine appointments help people get the quick care they need, and they've been associated with smaller health care costs, but there's a catch. Even in states that allow doctors to prescribe controlled medications, most require some sort of connection between the doctor and the patient. You must be under the professional's care in some way, meaning that you had an in-person appointment in the past. The Center for Connected Health Policy says states have a lot of control over telemedicine rules. But lawmakers must parse appointments and determine whether a digital visit really gives a doctor enough information about who you are, what's happening with your body, and what should come next. In most states, experts feel a telehealth visit just isn't enough for a controlled substance.
How to Skip an In-Person Visit
It may not be reasonable or even possible for you to go to the doctor whenever you need a prescription for an illness. And in some cases, you really can skip out on the appointment and get what you need. For example, some common prescriptions people need are not controlled substances.
Birth control
Antibiotics
Blood pressure drugs
Insulin
Cholesterol-lowering drugs

If you don't need a controlled substance, you have plenty of options open to you, including:
Telemedicine. According to the American Hospital Association, 76 percent of hospitals connect with patients via video or other technology. Typically, your health insurance company will set up a relationship with a network of doctors, and you'll contact that group when you need help. In a telemedicine visit lasting just a few minutes, you'll have a prescription to pick up. The provider you talk to will call it into your pharmacy of choice.
Pharmacies. Large chains like CVS employ nurse practitioners who can meet with you quickly, look up your history of prescriptions, and refill your supply if you're out. If you don't have a prescription already, you may not be able to access this help in all locations. But if you do and you've just run out of refills, this could be a good option.
Your doctor. It's hard to know how many physicians will authorize medications over the phone, says Mother Jones, but it's not uncommon for doctors to take calls from patients, hear their concerns, and write prescriptions. If you're dealing with an infection that's treated with antibiotics, this is especially common.

One thing you shouldn't do is buy medications online. Foreign websites offer a plethora of medications, and often, they claim they can sell you what you need with no prescription whatsoever. With one click of a button and a swipe of a credit card, you could get the pills you've been hoping for. If you use a system like this to buy a controlled substance (like a painkiller), you're breaking very serious laws, and you could end up in jail. If you've been caught before and this is your second offense, the fines can be swift and severe. You could also buy pills that contain completely different substances. You might think you're purchasing an antibiotic, for example, but the pill you’re holding might contain a narcotic. Take too much, and you could overdose and lose your life. Legislators know that consumers want to get medications without the hassle of a doctor's appointment, and proposals currently working through the system could help. The newsletter mHealth Intelligence suggests that the Trump Administration signed support for an act that would examine and/or adjust telemedicine prescribing laws. That could make it easier for you to get controlled substances at the end of a telemedicine visit with a doctor you've never met before. But the newsletter points out that legislation like this has been proposed and passed before, and nothing changed. That could happen again here, although legislators hope for something different.
Where Should You Start?
Many health insurance companies offer telehealth benefits to their subscribers. Often, you must register for the service before you need it, and there are fees and copayments involved. Call your health insurance company, and ask if you're eligible to contact a doctor via an online portal or chat. Find out how to sign up, and learn more about how much each visit will cost you. If you can, register for the service now. You can give the telehealth service the following information:
Age
Current medical conditions
Prescriptions
Allergies
Family health history
When you're sick or you need help, your telemedicine provider will have all of the information required to prescribe medications and otherwise help you to get better. Next, make sure you have a good relationship with a doctor in your community. Go to visit that provider every year for a checkup, and make sure you keep your prescription list current. If you get sick, your doctor might be willing to step in and help, even without an appointment, based on your history of work together. While no one wants to get sick and require medications, planning ahead can ensure that you don't add to an already stressful situation.
References
Therapeutic Drug Use. (January 2017). Centers for Disease Control and Prevention.
15-Minute Visits Take a Toll on the Doctor-Patient Relationship. (April 2014). Kaiser Health News.
Patients Give Doctors High Marks for Prescribing Antibiotics for Common Sniffles. (October 2014). National Public Radio.
New State Laws Allow Telehealth Prescriptions for Controlled Substances; Yet, Regulatory Obstacles Still Remain. (January 2018). Epstein Becker Green.
States Expand Telemedicine to Allow Prescribing of Controlled Substances. (July 2018). Modern Healthcare.
National Policy: Online Prescribing. Center for Connected Health Policy.
Fact Sheet: Telehealth. (February 2019). American Hospital Association.
One-Time Medication Renewal. CVS Pharmacy.
Should You Ask Your Doctor for Antibiotics Over the Phone? (January 2014). Mother Jones.
ATA Presses DEA to Loosen Telemedicine Restrictions for Prescribing. (January 2019). mHealth Intelligence.

Related Articles
How To Get Prescribed Adderall For ADHD Treatment. Getting an Adderall Prescription Online: Is It Possible?
How to get prescribed Adderall online? Is it possible...
How to Get a Finasteride Prescription Online
Finasteride is a medication that is used to treat...
What It Takes to Get a Phentermine Prescription Online
Phentermine is a prescription weight-loss pill that can...
How to Get a Desoxyn Prescription Online
Patients with attention deficit hyperactivity disorder...
